It was February 2020, just before one of the biggest global pandemics struck, that I attended the IACR as a research assistant. It was my first official conference and it is safe to say ‘Imposter Syndrome’ was my main feeling going down to Galway on the train. Fast forward 2 years and my feelings travelling to IACR 2022 in Cork could not be more different. It is amazing what starting a PhD during a pandemic can do for your confidence and skills as a researcher – a sink or swim moment if there was ever one. My first IACR in Galway was one to remember surrounded by like-minded scientists, all brimming with new ideas and exciting discoveries. As such, I had high hopes for IACR 2022. And it did not disappoint.

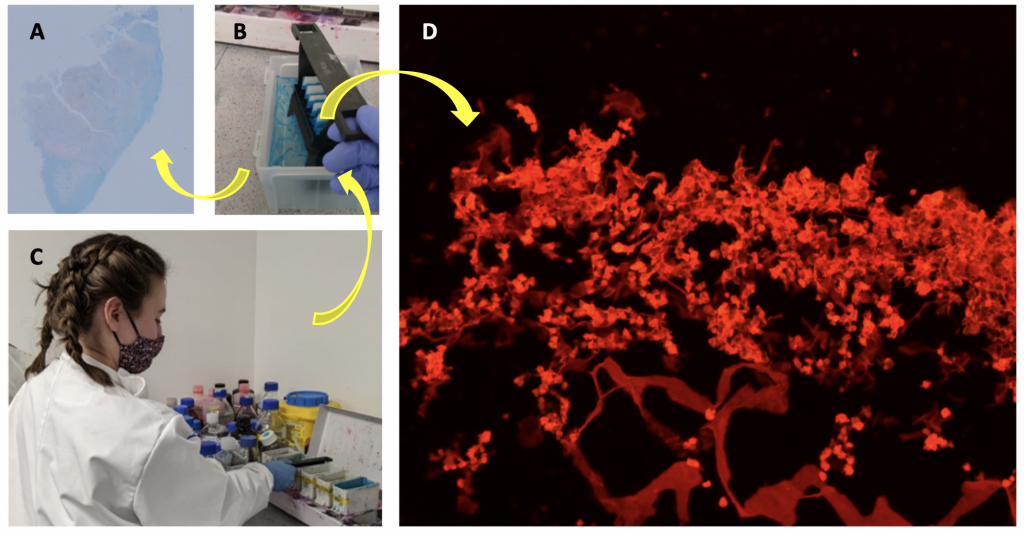
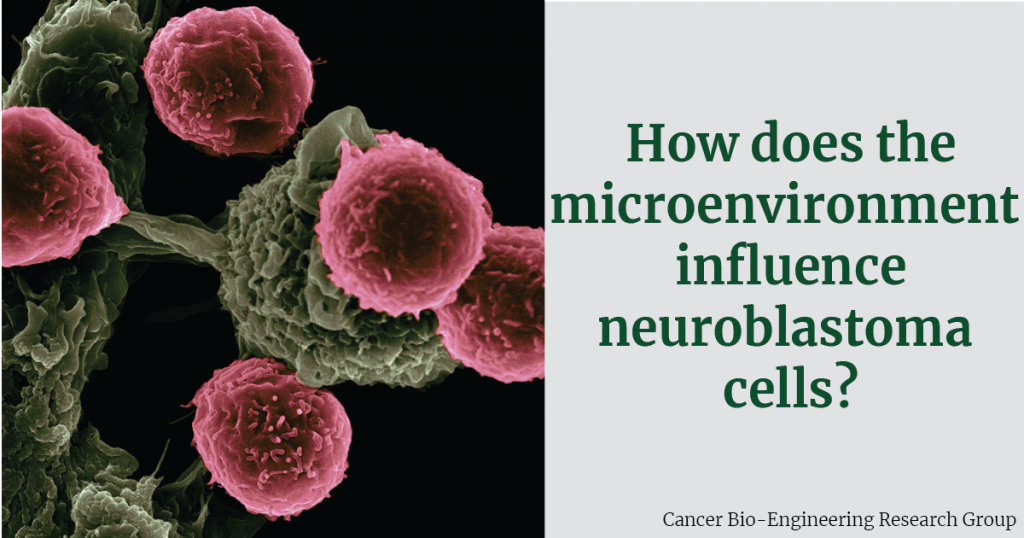
My PhD project focuses on the development of a vaccine to treat neuroblastoma so I was very excited to hear talks from some of the leading experts in vaccine research, both in industry and academia. I gained so much from hearing these experts discuss their research but also discussing other important topics like career progression and how to keep a work/life balance in research. It was refreshing to hear that as scientists we don’t have to (and shouldn’t) work ourselves to the bone 24/7 to be successful. As a young scientist planning to continue into academic research, this left a lasting impression on me. To top off what was already a hugely beneficial conference for me, my poster was shortlisted for a prize. I was shocked, delighted and excited all-in-one. Starting my PhD during a pandemic was not without challenges. Delays in deliveries, delays getting trained on equipment and multiple lockdowns led to what felt like (for me) quite a disjointed start. For my research to be shortlisted by experts was, to be honest, a relief. To know that my work stood out was extremely important to me and that all the hard work does pay off. When my name was called out at the Gala dinner as a Poster Prize Winner, all the doubts that I had (doubts that we all have as scientists) disappeared. I felt very proud and very grateful that my research was recognised at that level. There is no doubt that in-person conferences give a huge boost to young researchers, and I really look forward to presenting my work at the next IACR meeting.
Written by Ellen King