We are delighted to provide training and contribute to neuroblastoma research through the Mac4Me Doctoral Network Programme. Mac4Me is a 48-month project that addresses both technical and social challenges in cancer metastasis. It focuses on three tumour types that show poor response to current immunotherapies: neuroblastoma, breast, and prostate cancer. These tumour types reflect cancer development across a person’s lifetime and share metastatic disease spreading to the brain, bone, and liver.
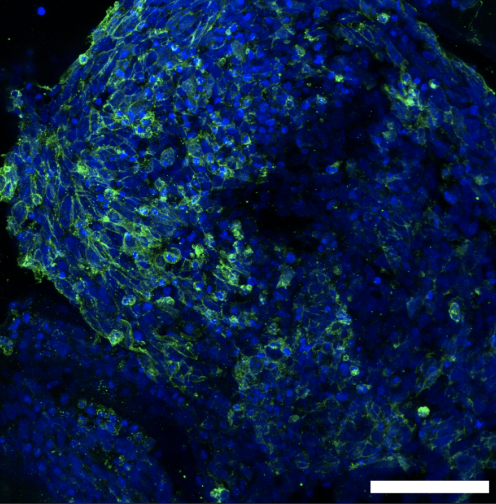
Working alongside researchers and patients, the network will train 18 Doctoral Candidates to study the tumour microenvironment at metastatic sites, with a particular focus on the macrophage immune cell population. It will combine organ-on-chip technology with microfluidic systems to investigate early cell-cell and cell-matrix interactions during tumour invasion. Mac4Me will move beyond traditional “thinking in boxes” approaches by integrating bioinformatics and Artificial Intelligence solutions with real-world clinical data. The project will focus on patient experiences and translate scientific advances into meaningful outcomes.
We are very proud to train two out of 18 Doctoral Candidates, building upon the expertise of Drs Ian Woods, Adrian Dervan and Prof Fergal O’Brien in biomaterials and 3D bioprinting and Dr Olga Piskareva in neuroblastoma biology and 3D in vitro cancer models.