Once I mentioned the importance of the publication track record for a career in science. My team has been productive despite the COVID pandemic. Two review articles were published.
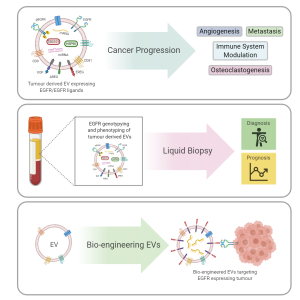
The first was a review written by Tom and published in Cancers focusing on the small extracellular vesicles produced by cancer cells that can transfer various growth signals to the tumour microenvironment aka neighbourhood and promote tumour expansion. The signal in focus was a protein called epidermal growth factor receptor (EGFR). It contributes to the healthy fitness of many different cells in the body. However, many cancer cells produce an excess of this protein giving them an advantage of growth over normal cells. Increased EGFR can be seen in breast, lung, glioblastoma and head and neck cancers.
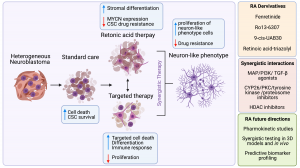
The second review has been published in Journal of Personalized Medicine on March, 16th. Originally, it was a small review project for Nadiya, a medicine student, last summer. However, it became a big one with all data systematically collected, analysed and condensed. The focus of this review was on Retinoic Acid (RA), widely known as Vitamin A and its role in neuroblastoma. RA plays a vital role in human development. The main feature of RA is to push neuroblastoma cells to become neuron-like cell stopping their aggressiveness and cancer fate. So, we wanted to know more about the ongoing research both in the labs and the clinic. We reviewed primary research articles reporting basic and translational findings as well as clinical trials. Hopefully, it would help other researchers to get a full picture of this topic and a structured resource of experimental models and drugs tested.


 This was our 2nd time attending the OLCHC Research & Audit Day on May 25th, 2018. The conference provides a great forum for paediatric clinicians to share and update knowledge across different specialties through talks and poster presentations. It is insightful for basic biomedical researchers like us to see other perspectives.
This was our 2nd time attending the OLCHC Research & Audit Day on May 25th, 2018. The conference provides a great forum for paediatric clinicians to share and update knowledge across different specialties through talks and poster presentations. It is insightful for basic biomedical researchers like us to see other perspectives.